Rethinking HRT: Dispelling the Breast Cancer Myth for a Vibrant Healthspan
Introduction: The Persistent Shadow of Fear
The whispers started quietly, then grew into a roar: Hormone Replacement Therapy (HRT) causes breast cancer. This fear, ignited decades ago, has cast a long shadow, leading countless women to needlessly suffer through debilitating perimenopausal symptoms in silence. The narrative became so dominant that it obscured a vital truth: the science has evolved, and with it, our understanding of HRT's true role in a woman's health journey. At Cacti Fit, we're here to cut through the noise and equip you with the accurate, science-backed information you deserve. You've navigated countless challenges in life with resilience; it's time to apply that same strength to your body and well-being. This article isn't about promoting HRT for everyone, but about dispelling a pervasive myth, empowering you with knowledge, and fostering a proactive mindset to truly thrive through life's transitions and not just endure them. It's about recognizing that ignoring treatable medical issues is not a badge of honor, nor a situation to be ashamed of, and that tools exist to help you live the vibrant, full life you're capable of.
The Original WHI: A Landmark Study, Misunderstood
The Infamous 'Black Box' Warning
Initially a symbol of alarming risk, subsequent re-analysis has shown a more nuanced truth behind its stark pronouncements, which we delve into next.
To understand where we are, we first need to confront the past. In 2002, the Women's Health Initiative (WHI) study, a massive, federally funded undertaking, rocked the medical world and the lives of millions of women. The initial findings on its combined estrogen-progestin arm delivered a stark blow: the study was halted early, seemingly out of an abundance of caution, due to reported increased risks of breast cancer, heart disease, stroke, and blood clots. The reaction was immediate and seismic. Doctors rapidly pulled women off HRT, pharmaceutical companies faced massive lawsuits, and the media, as it often does, amplified the most alarming headlines. The fear became palpable, leading to the infamous "black box" warning that still haunts HRT prescriptions today. For a time, it felt like the scientific community had spoken, definitively closing the book on HRT as a viable option for many women. But, as with many things in life, the truth behind such a complex issue is rarely so simple. The WHI was indeed a landmark study, an amazing undertaking and a rich dataset, but its initial communication might just be the biggest science communication blunder of its time.
Understanding Risk: Relative vs. Absolute
Part of that communication problem stems from how risk is often presented to the public. Let’s consider this: Imagine you hear that a certain activity increases your risk of something bad happening by 50%. Sounds terrifying, right? That’s relative risk at work; it tells you how much more likely something is to happen compared to a baseline. It's great for dramatic headlines; fear and controversy get eyeballs, and there you have it. But what if the original risk was incredibly tiny to begin with? That’s where absolute risk comes in. Absolute risk tells you the actual likelihood of an event occurring. For instance, if the original risk was 1 in 10,000, and a "50% increase" means it's now 1.5 in 10,000, the absolute increase is still incredibly small. This nuance was largely lost in the initial WHI reporting. The headlines screamed about increased percentages, overshadowing the minuscule actual changes in overall risk for most women, especially those in their early perimenopausal years. This oversight, whether intentional or not, caused widespread panic and cemented a fear-based narrative that persists to this day.
Relative risk
Imagine you have one apple, and then you get a '50% increase' in apples. You now have one and a half apples. This visually demonstrates the proportional increase from a small starting point. This metric, while technically correct, can make a small change seem very dramatic.
Absolute Risk
Imagine a large oak barrel filled with 10,000 red apples, and only 2 of them is rotten. That's your baseline risk. Now, let's say a 'new factor' causes a '50% increase' in rotten apples. For the barrel of green apples, that means you'd now have 3 rotten apples per 10,000. While '50% increase' sounds big, the actual number of additional rotten apples is still tiny. This second visual helps to truly grasp the actual change in likelihood, not just the proportional change.
The WHI Re-analysis: Unveiling Critical Nuances and True Risk
The initial conclusions from the WHI, while impactful, missed crucial nuances. Science, at its best, is about continuous inquiry and refinement. Thankfully, dedicated researchers didn't let those initial headlines be the final word. A meticulous re-analysis of the WHI data, alongside other extensive studies, has unveiled a far more sophisticated and often reassuring picture of HRT. This re-evaluation is precisely why we must challenge the prevailing wisdom that persists in its lag.
Then
In the early 2000s, headlines screamed. The initial interpretation of the Women's Health Initiative study ignited fear and confusion, leaving many women bewildered by conflicting information about their health.
Now
The science has evolved. Today's women, armed with new research and a desire for deeper understanding, approach their health journeys with inquisitive intrigue, ready to uncover the full, nuanced truth.
The Timing Hypothesis: HRT is Not One-Size-Fits-All
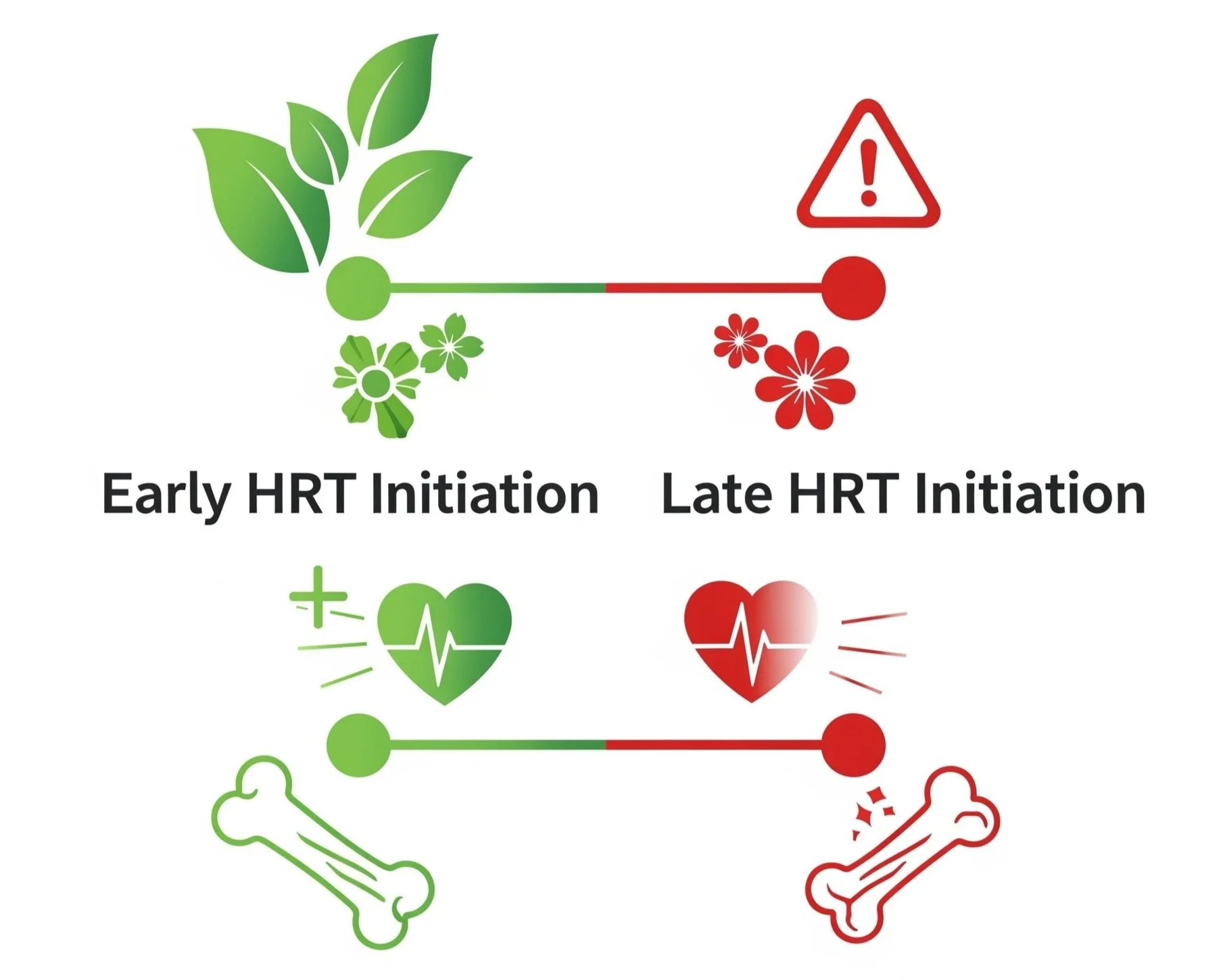
The Timing Hypothesis
When it comes to HRT, when you start matters. This graphic illustrates that initiating HRT earlier in your perimenopausal journey can lead to a more favorable balance of benefits and risks, aligning with a path of vitality and sustained health.
Perhaps the single most critical breakthrough from the re-analysis is the "Timing Hypothesis." This concept highlights that the safety and benefits of HRT are heavily dependent on when it's initiated relative to menopause onset. If HRT is started in younger women (typically under 60) or within 10 years of their last menstrual period, the benefits for managing symptoms like hot flashes, night sweats, and genitourinary syndrome of menopause (GSM), along with bone density, generally outweigh the risks. In this "window of opportunity," the cardiovascular risks are actually lower, and there's even potential for reduced all-cause mortality. Conversely, initiating HRT later (over 60 or more than 10 years post-menopause) presents a less favorable risk-benefit profile. This isn't a blanket "safe" or "unsafe" statement; it's about the strategic application of a powerful tool.
Formulation Matters: Not All HRT is Created Equal
The initial WHI study predominantly used a specific type of combined HRT: conjugated equine estrogens with synthetic medroxyprogesterone acetate (MPA). But the world of HRT is far more diverse than a single pill.
Estrogen Type: For women who have had a hysterectomy and therefore take estrogen-alone therapy, the re-analysis shows no increased risk of breast cancer. In fact, some evidence suggests a potentially reduced risk. This is a critical distinction often lost in the broad "HRT causes breast cancer" narrative.
Progestin Type (Your Pharmacological Edge): This is where the devil is truly in the details. The synthetic progestin (MPA) used in the original WHI is indeed linked to a small, duration-dependent increased risk of breast cancer when combined with estrogen. However, modern understanding and observational studies suggest that micronized progesterone (which is bioidentical to the progesterone your body naturally produces) may carry a lower or even no increased risk. Furthermore, micronized progesterone can act as a 5α-reductase inhibitor, potentially influencing DHT levels and offering an anti-androgenic effect. This nuanced understanding of how different progestins interact with your body's systems is a testament to the advancements in endocrinology and pharmacology that shouldn't be overlooked.
Delivery Method Matters: Oral, Transdermal, and Other Routes
Beyond the pill
HRT delivery methods matter. This visual highlights common options including oral pills, transdermal patches or gels, and injectables. Each method interacts with your body differently, impacting factors like liver metabolism and systemic absorption, making the choice a crucial part of a personalized approach.
How hormones are delivered to your body also plays a significant role in their safety profile.
Oral Estrogen: When estrogen is taken orally, it undergoes "first-pass metabolism" in the liver. This process can increase clotting factors, which in turn slightly elevates the risk of venous thromboembolism (VTE) and stroke, especially in older women initiating therapy. Oral estrogen can also significantly reduce bioavailable testosterone by increasing Sex Hormone Binding Globulin (SHBG). If you're struggling with low libido, for example, oral estrogen could inadvertently make that worse.
Transdermal Estrogen: In contrast, transdermal estrogen (delivered via patches, gels, or sprays applied to the skin) largely bypasses the liver's first-pass metabolism. This leads to a significantly lower risk of VTE and stroke, making it a preferred route for many women. It also avoids the SHBG-mediated reduction in bioavailable testosterone.
Injectable Estrogen (IM or SubQ): While less common for general HRT prescriptions in women, injectable forms (intramuscular or subcutaneous) also bypass first-pass liver metabolism, offering similar advantages to transdermal routes in terms of VTE and SHBG impact. For those who overcome initial apprehension, self-injection can become a simple, routine method of delivery, akin to brushing your teeth after a few tries.
Beyond Breast Cancer: HRT as a Tool for Healthspan
While the breast cancer narrative dominated, it's vital to put the risk into perspective. Yes, combined estrogen-progestin therapy carries a small, duration-dependent increased risk of breast cancer incidence, particularly with synthetic progestins. However, it is crucial to understand that this increased incidence of breast cancer does not necessarily translate to an increased risk of death from breast cancer. This distinction between being diagnosed with a condition and dying from it is paramount and often completely missed in public discourse.
HRT is a powerful tool to address debilitating perimenopausal symptoms such as hot flashes, night sweats, and the often-ignored genitourinary syndrome of menopause (GSM). Beyond symptom relief, HRT plays a critical role in maintaining bone density, actively working to prevent or manage osteoporosis. When initiated appropriately within that "window of opportunity," it can even support cardiovascular health and reduce all-cause mortality. This isn't about ignoring risks; it's about making informed, strategic decisions. Eventually we all die, and more power to you if you think you know what happens next. After some point, when we are really young, we are constantly aging, nudging ever closer. But pretending there's nothing you can do to optimize your healthspan, the vibrant, active years of your life, is simply a choice to suffer unnecessarily. Fitness, nutrition, and, yes, strategically chosen HRT, are amazing tools to facilitate that process. If right now perhaps you have been sticking your head in the sand like an ostrich from the felt sense of overwhelm, I invite you to take meaningful action to live the life you know you want to.
Beyond Belief: Act & Optimize Healthspan
This is your potential!
Beyond the outdated fears, embracing informed action like strategic HRT, alongside fitness and nutrition, empowers you to live a vibrant, attractive, and truly full life. This is what optimizing your healthspan looks like.
We've unpacked the science, clarified the risks, and hopefully, started to dismantle the fear surrounding HRT. Now, let's address the mindset that often keeps women from seeking the relief and vitality they deserve. There is nothing noble in suffering silently through hot flashes, sleepless nights, joint pain, or the profound changes that perimenopause can bring. Choosing to endure these symptoms without exploring effective, evidence-based treatments is not a sign of strength; it's a choice to limit your own healthspan and quality of life.
The idea that one might become "dependent" on HRT is another fear-based narrative that needs to be challenged. This is not about addiction; it's about providing your body with what it needs to function optimally as its endogenous hormone production changes. The fear of dependence leads to unnecessary suffering, keeping women from a tool that could significantly enhance their well-being. Consider oral contraceptives: they are, in a very real sense, a form of hormone replacement therapy. They suppress your endogenous hormone experience and introduce exogenous analogs to achieve a desired physiological outcome. We accept this for birth control, yet balk at the idea of using hormones to manage the later stages of our reproductive lives. The principle of hormonal modulation is not new or inherently frightening.
A significant barrier to women receiving appropriate care is the knowledge gap that persists within the medical community itself. Many primary care physicians, and even a surprising number of endocrinologists, OB/GYNs, and urologists, are simply not as informed on modern HRT guidelines and nuances as they should be. This unfortunate reality means countless perimenopausal patients are underserviced, dismissed, or given outdated advice. This contributes directly to the lament of "Why did no one tell me!?" when women finally discover the options available to them. This is your moment to act. While fitness and nutrition are foundational pillars that will absolutely increase your longevity and, more importantly, your healthspan, HRT is an amazing tool to facilitate that process. I know this stuff can feel overwhelming, but I know you are not an ostrich, so lift that head of yours! I invite you to take meaningful, informed action to live the vibrant life you know you want to. Your body is changing, and that's a fact. How you choose to navigate those changes, armed with accurate information and the right tools, is entirely within your control.
Conclusion: Your Right to Informed Health and a Thriving Life
We've journeyed through the complexities of the Women's Health Initiative, from its initial, widely misunderstood findings to the crucial re-analysis that has illuminated a far more nuanced and often reassuring truth about Hormone Replacement Therapy. The core message is clear: HRT, when initiated appropriately and with the right formulations, is a valuable, safe, and effective tool for most women navigating perimenopause. The pervasive fear linking HRT unequivocally to breast cancer, particularly to an increased risk of death, is largely a relic of outdated interpretations and flawed communication.
Your health journey is yours to own, and that includes the right to accurate, evidence-based information. It is time to move beyond the fear-based narratives and the societal pressure to silently endure. Embrace the knowledge that HRT can significantly alleviate debilitating symptoms, support bone density, and even contribute positively to cardiovascular health, especially when timed correctly within your life's transitions.
Do not settle for suffering. Do not accept outdated advice. Seek out healthcare providers who are informed on the latest science in women's health and HRT. Combine this informed approach with the foundational pillars of fitness and nutrition, which Cacti Fit champions. These are the powerful tools at your disposal to not just survive perimenopause, but to truly thrive through it and optimize your healthspan for decades to come. You have the power to live a vibrant, full life. It's time to take control, make informed choices, and demand the care that empowers you to flourish.